Common histopathology terms
HISTOPATHOLOGY TERMS DESCRIBED
Hyperplasia
Acanthosis
Hyperkeratosis
Atrophy
Acantholysis
Metaplasia
Dysplasia
Epithelial invasion into connective tissue
Rete ridges
HYPERPLASIA
Hyperplasia is used to describe an increase in number of cells which would result in an increase in size or thickness of a tissue or organ.
In the oral mucosa, hyperplasia can manifest in the
epithelial component; Eg --> frictional keratosis, leukoplakia.
connective tissue component. Any connective tissue component, like the endothelial cells of blood vessels, fibroblasts etc could become hyperplastic. Eg --> Fibroma (fibrous hyperplasia), pyogenic granuloma (hyperplastic granulation tissue), denture epulis (fibrous hyperplasia).
💡Note
Understand that hyperplasia is distinct from neoplasia. Neoplasia is an abnormal increase in the number of cells (excess proliferation) as a result of mutation, causing impairment in control measures keeping a check on the proliferation of cells. ACANTHOSIS
Acanthosis is a term reserved for hyperplasia of the spinous layer.
“Acanth” in acanthosis is derived from the Greek word “akantha” meaning “thorn” or “prickle” (spinous layer is also called the prickle cell layer) and “osis” refers to an “increase”.
HYPERKERATOSIS
Hyperkeratosis is an increase in the corneal layer or stratum corneum.
Usually in epithelial lesions (especially white lesions), there is hyperkeratosis accompanying hyperplasia of the epithelium.
Hyperkeratosis could be described as being
Hyperorthokeratotic --> increase in orthokeratin (corneal layer)
Hyperparakeratotic --> increase in parakeratin (corneal layer)
The difference between orthokeratin and parakeratin is that parakeratin would show pyknotic nuclei and orthokeratin would not.
Examples of lesions manifesting hyperkeratosis --> White lesions like leukoplakia, verrucous carcinoma, verrucous hyperplasia, tobacco pouch keratosis, nicotine stomatitis, frictional keratosis (cheek, tongue, lips and alveolar ridges).
💡Know Thy Facts
Leukoplakia or other white lesions for that matter, appear white because of the thickened surface keratin layer and the hyperplastic epithelium. This thickened abnormal keratin layer evenly reflects the visible light spectrum (as opposed to being permeable to visible light and the red spectrum being reflected by the connective tissue). This clinically masks the vascularity (redness) of the underlying connective tissue making it appear white!ATROPHY
Atrophy is a decrease in size of tissue/organ, either due to a decrease in size of cells or due to a decrease in number of cells.
Examples of lesions manifesting atrophy:
Erythroplakia shows epithelial atrophy. The epithelium is reduced in thickness (very thin, no rete ridges) and there is no keratosis (hence appears red).
Oral lichen planus, atrophic type --> The epithelial layer is thinned with no rete ridges.
ACANTHOLYSIS
Acantholysis is the loss of attachment between epithelial cells.
During acantholysis, there is a breakdown of the intercellular connections between epithelial cells, called desmosomes.
This results in epithelial cells losing their cohesion, forming intra-epithelial clefts and blisters (also known as an intra-epithelial split).
The free floating spinous cells within the split lose their polygonal shape and become spherical/round. These are called Tzanck cells.
Examples of lesions exhibiting acantholysis --> pemphigus vulgaris, erythema multiforme, herpes simplex vesicles.
METAPLASIA
Metaplasia is a process where a differentiated adult cell type is replaced with another cell.
Take salivary gland lesions for example:
In necrotizing sialometaplasia, the minor salivary gland ducts undergo a squamous metaplasia, where the columnar or pseudo-stratified columnar cells of the ducts are replaced by squamous cells.
In pleomorphic adenoma neoplastic myoepithelial cells, ductal cells or both may undergo mesenchymal metaplasia to give rise to varied tissue components like chondroid, myxoid, chondromyxoid and very rarely, osseous and adipose tissue.
DYSPLASIA
The term “dysplasia” denotes the abnormal/disordered production or development of tissues.
When referring to “epithelial dysplasia”, the term is used to designate atypical characteristics of the epithelium (indicating malignant risk) under the microscope.
Epithelial dysplasia is characterized by --> a) cellular atypia and b) disruption in the architectural orientation of the tissue.
Oral potentially malignant disorders (OPMDs) like leukoplakia or erythroplakia may (or may not) show epithelial dysplasia histopathologically.
Assessing the presence and grading of epithelial dysplasia histologically, is still considered gold standard for predicting the malignant transformation of OPMDs.
WHO 2017 classification of oral epithelial dysplasia advocates the grading of dysplasia as mild, moderate and severe.
(Refer topic “Epithelial Dysplasia” for more details)
💡Note
The term “dysplasia” in lesions like fibrous dysplasia or cemento-osseous dysplasia, refers to the abnormal/ disordered production and development of bone. It does not refer to or signify the presence of “atypia” or “pre-malignant” features that are described in potentially malignant mucosal lesions like leukoplakia!INVASION OF EPITHELIUM INTO CONNECTIVE TISSUE
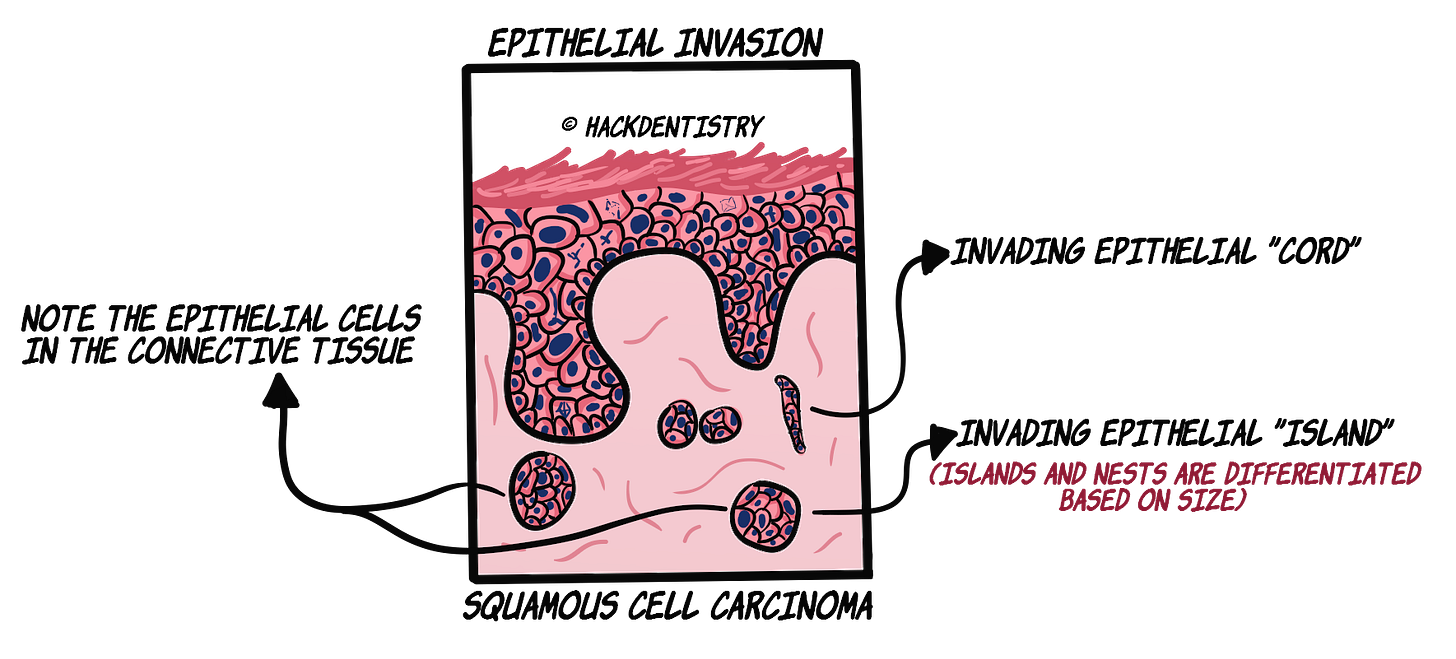
Invasion of epithelium into the connective tissue is seen in epithelial carcinomas like oral squamous cell carcinoma.
This is a description used when the epithelium proliferates within the connective tissue.
Normal -->The epithelium is clearly demarcated from the connective tissue by a basement membrane or a basal lamina.
Carcinoma --> In epithelial carcinomas, the malignant dysplastic epithelium penetrates the basement membrane and enters the connective tissue.
The “invading” atypical epithelial cells would then proliferate in the connective tissue to become small cords, nests or islands of (dysplastic) cells.
The “invading” cords, nests or islands of malignant epithelial cells would extend deeply, penetrate and destroy other connective tissue components like adipose tissue, muscle, blood vessels or bone.
Only when the epithelial cells have invaded the connective tissue is the lesion branded a “carcinoma”. A dysplastic epithelium without invasion is termed “epithelial dysplasia”.
💡Note
An exception to this rule is “Verrucous carcinoma” where there is no connective tissue invasion by the epithelium.
A characteristic feature of verrucous carcinoma is its endophytic growth pattern --> the lesional epithelium, with an intact basement membrane, pushes deep into the connective tissue (but does not invade the connective tissue like squamous cell carcinoma) and grows beyond the level of the basement membrane of the adjacent normal epithelium.(Refer topic "Verrucous carcinoma" for more details)
RETE RIDGES
In the oral mucosa and skin, epithelial extensions called rete ridges or rete pegs interlock with the underlying connective tissue papillae.
Hence the interface between the epithelium and connective tissue in the oral mucosa is undulating or wavy.
The epithelial rete ridges may assume characteristic shapes in certain oral lesions.
SAW TOOTH RETE RIDGES
“Saw tooth” rete ridges are classically seen in oral lichen planus and lichenoid reactions/lesions.
The normal “U-shaped” rete ridges become pointed resembling a “saw tooth”, hence the name.
The rete ridge, in these lesions, assumes this shape due to the basal cell degeneration of the epithelium by the subjacent inflammatory cells.
DROP SHAPED RETE RIDGES
Drop shaped or bulbous rete ridges may be seen in lesions showing dysplasia.
In fact, “drop shaped rete ridge” is considered to be an important dysplastic feature (architectural change) (refer Table in “Dysplasia” section).
Rete ridges assume this shape due to excessive proliferation of basal cells.
ELEPHANT'S FOOT RETE RIDGES
In verrucous carcinoma, rete ridges are elongated, thick and bulky, and push into the adjacent connective tissue.
They are described as having an “elephant’s foot” appearance.
✅HIGHLIGHTS - VIVA & ENTRANCE EXAM PERSPECTIVE
Hyperplasia is used to describe an increase in number of cells which would result in an increase in size or thickness of a tissue or organ. Eg --> a) epithelial hyperplasia --> leukoplakia, frictional keratosis b) fibrous hyperplasia --> fibroma.
Acanthosis is a term reserved for hyperplasia of the spinous layer.
Hyperkeratosis is an increase in the corneal layer or stratum corneum. Eg -> white lesions like leukoplakia, verrucous carcinoma, tobacco pouch keratosis.
Atrophy is a decrease in size of tissue/organ, either due to a decrease in size of cells or due to a decrease in number of cells. Eg --> erythroplakia, atrophic oral lichen planus.
Acantholysis is the loss of attachment between epithelial cells. This results in epithelial cells losing their cohesion, forming intra-epithelial clefts and blisters (also known as an intra-epithelial split). Eg --> Pemphigus vulgaris, erythema multiforme, herpes simplex.
Metaplasia is a process where a differentiated adult cell type is replaced with another cell. Eg --> squamous metaplasia of ducts in necrotizing sialometaplasia.
The term “dysplasia” denotes the abnormal/disordered production or development of tissues. When referring to “epithelial dysplasia”, the term is used to designate atypical characteristics of the epithelium (indicating malignant risk) under the microscope.
Epithelial invasion is seen in epithelial carcinomas like oral squamous cell carcinoma. The malignant dysplastic epithelium penetrates the basement membrane and enters the connective tissue. An exception to this rule is “Verrucous carcinoma” where there is no connective tissue invasion by the epithelium.
“Saw tooth” rete ridges are classically seen in oral lichen planus and lichenoid reactions/lesions.
Drop shaped or bulbous rete ridges may be seen in lesions showing dysplasia.
In verrucous carcinoma, rete ridges are elongated, thick and bulky, described as having an “elephant’s foot” appearance.
📖REFERENCES AND FURTHER READING
Kumar V, Abbas AK, Fausto N, Aster JC. Robbins and Cotran - Pathologic Basis of Disease.8 th ed. Saunders Elsevier; 2010.
Neville BW, Damm DD, Allen CM, Chi A. Oral and Maxillofacial Pathology. South Asian ed. Elsevier; 2016.
Rajendran R, Sivapathasundaram B. Shafer’s Textbook of Oral Pathology. 7th ed. Elsevier; 2012.
Regezzi JA, Sciubba JJ, Jordan RCK. Oral Pathology: Clinical Pathologic Correlations. 5 th ed. Elsevier; 2007.
Sapp JP, Eversole LR, Wysocki GP. Contemporary Oral and Maxillofacial Pathology. 2 nd ed. Mosby; 2004.
Seshadri D, Kumaran MS, Kanwar AJ. Acantholysis revisited: back to basics. Indian J Dermatol Venereol Leprol. 2013 Jan-Feb;79(1):120-6.
Ranganathan K, Kavitha L. Oral epithelial dysplasia: Classifications and clinical relevance in risk assessment of oral potentially malignant disorders. J Oral Maxillofac Pathol. 2019;23(1):19–27.
Jerry E. Bouquot, Paul M. Speight, Paula M. Farthing. Epithelial dysplasia of the oral mucosa—Diagnostic problems and prognostic features.Current Diagnostic Pathology.2006;12: 11–21.
Brannon RB, Fowler CB. Benign fibro-osseous lesions: a review of current concepts. Adv Anat Pathol. 2001;8(3):126-43.
Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36(10):575-80.
Thomas GJ, Barrett AW. Papillary and verrucous lesions of the oral mucosa. Diagnostic histopathology.2009;15(6):279-285.