Diabetes and periodontitis - The two way relationship
🎥HackDentistry - YouTube
A quick shout out! Here's a “video version” of the article.
DIABETES'S EFFECT ON PROGRESSION OF PERIODONTITIS
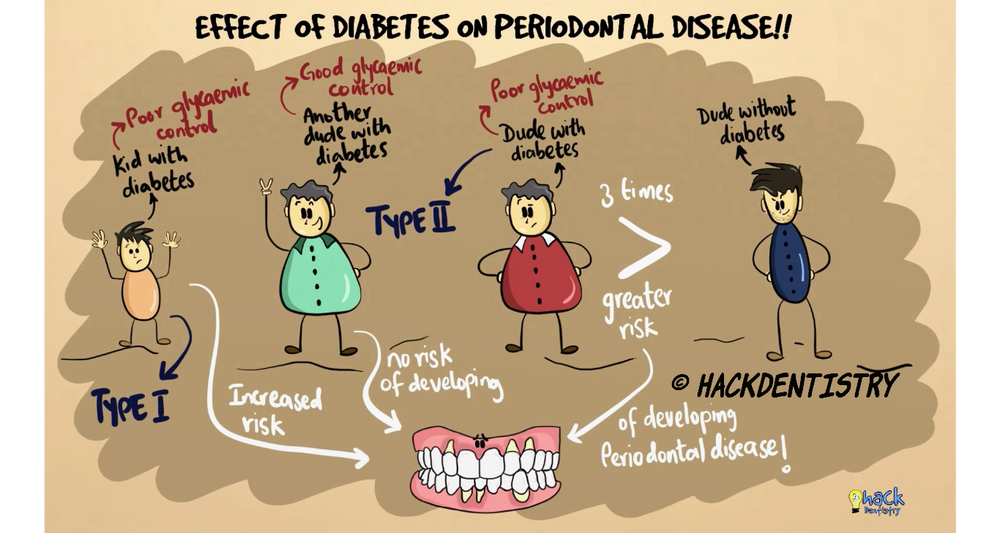
It is reported that individuals with diabetes have a 3 fold increased risk of developing periodontal disease than individuals without diabetes.
However, it has to be remembered that research implicates poorly controlled diabetes as a risk factor for periodontal disease as opposed to diabetic patients with good glycaemic control who have been reported not to have any significant risk of developing periodontitis.
It is also established that both types of diabetes, type I and type II are at an increased risk of developing periodontal disease.
Poorly controlled diabetes by itself does not directly cause periodontitis, but affects how periodontal tissues respond to local factors like plaque, thereby creating an environment conducive for the development of the disease.
Research initially focused on the influence of diabetes on the oral microbial flora. But it was found that there was not much difference in the composition of the microbial flora in the periodontally diseased sites of individuals with and without diabetes.
There is lack of sufficient evidence to implicate diabetes in affecting the oral microbial composition which may increase the risk of developing periodontitis.
ALTERED IMMUNO-INFLAMMATORY RESPONSE
Neutrophils in diabetics have defective adherence, chemotaxis and phagocytosis. This may lead to survival and proliferation of microbes in the periodontal tissues further aggravating periodontitis.
In general, monocytes and macrophages apart from phagocytosing microbes also release pro-inflammatory cytokines like TNF-α and IL-1β.
It has been reported that patients with poorly controlled diabetes have an increased pro-inflammatory cytokine load. Monocytes and macrophages in diabetes patients have been reported to be hyper-responsive, releasing more than usual TNF-α and IL-1β (pro-inflammatory cytokines) leading to excessive periodontal tissue breakdown!
ADVANCED GLYCATION END PRODUCTS (AGEs)
Accumulation of advanced glycation end products abbreviated as AGEs, is one of the most important reasons for increased periodontal disease risk in diabetes patients.
AGEs could influence periodontal destruction by altering collagen metabolism and the immuno-inflammatory response.
In the hyperglycaemic state, AGEs form and accumulate in excess.
These end products interfere with normal collagen metabolism. They form cross links in collagen, thereby making them difficult to be repaired or replaced.
This results in accumulation of bad/damaged collagen for long periods, since they cannot be repaired or replaced normally.
Hence diabetics have aged unhealthy collagen that is susceptible to easy breakdown and has poor healing/self repair capacities.
Immuno-inflammatory alterations
AGEs interact with cell surface receptors called “receptor for advanced glycation end products” abbreviated as RAGE on inflammatory cells like monocytes and macrophages.
This AGE-RAGE interaction can cause an increased production of free radicals like reactive oxygen species (ROS) and pro-inflammatory cytokines like TNF-α and IL-1β all of which cause periodontal tissue destruction.
HOW DOES PERIODONTITIS AFFECT GLYCAEMIC CONTROL?
It is also now known that periodontitis may have an effect on the glycaemic control of individuals.
In fact, it is established that severe periodontitis can not only worsen the glycaemic control of diabetes patients but also increase the risk for non-diabetics to develop the disease.
Increasing Insulin resistance
One of the major effects of chronic inflammation is increasing insulin resistance. The more the insulin resistance, the more it is difficult for sugar to enter the tissues, thereby increasing blood sugar.
Periodontitis is a result of persistent chronic inflammation in the periodontal tissues. The saliva and gingival crevicular fluid of individuals with chronic periodontitis are known to show increased pro-inflammatory cytokine levels like TNF-α and IL-1β.
This dysregulated inflammatory environment could aggravate insulin resistance.
Chronic periodontitis hence has the potential to increase insulin resistance by nature of its inflammatory profile.
Clinical trials have also shown Hb1AC levels in diabetics to reduce by 0.36% after periodontal treatment. Periodontal therapy has shown to reduce pro-inflammatory cytokine levels in the serum, which could possibly lead to improvements in the glycaemic control in patients with diabetes.
📚 Study resources on our website
📖REFERENCES AND FURTHER READING
Chapple ILC, Genco R, and on behalf of working group 2 of the joint EFP/AAP workshop. Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol 2013; 40 (Suppl. 14): S106–S112.
Taylor JJ, Preshaw PM, Lalla E. A review of the evidence for pathogenic mechanisms that may link periodontitis and diabetes. J Clin Periodontol 2013; 40 (Suppl. 14): S113–S134.
Mealey BL. Periodontal disease and diabetes. A two-way street. J Am Dent Assoc. 2006 Oct;137 Suppl:26S-31S.
Preshaw PM, Alba AL, Herrera D, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55(1):21-31
Wu YY, Xiao E, Graves DT. Diabetes mellitus related bone metabolism and periodontal disease. Int J Oral Sci. 2015;7(2):63-72.
Newman MG, Takei H, Klokkevold PR, Carranza FA. Carranza’s Clinical Periodontology. 10 th ed. Elsevier; 2009.